Championing perinatal mental health for all

Overview
Creating Community
Kimberly Wong was an accomplished lawyer and new mother when she experienced a debilitating mental illness. Postpartum depression struck her after the birth of her daughter, and though she was well-resourced, she found that there was a lack of support and community for those living with perinatal mood disorders (PMDs). That’s why she founded Maternal Mental Health NOW (MMHN), formerly known as the Los Angeles County Perinatal Mental Health Task Force.

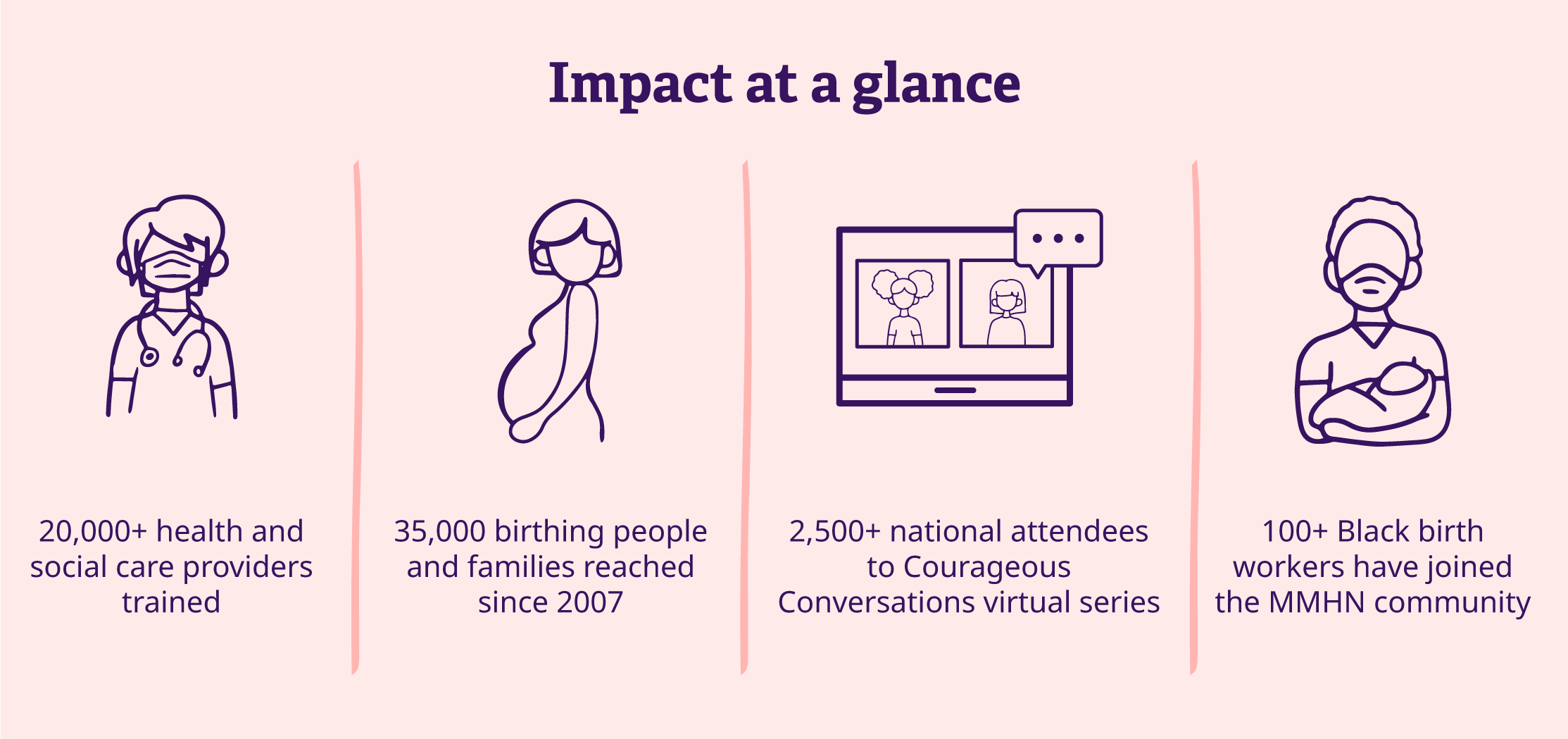
Since 2007, MMHN has served the Los Angeles community, working to increase awareness and access to care for all families affected by PMDs. PMDs affect 25% of birthing people in Los Angeles, according to a 2018 survey.
MMHN relies on the help of donors, volunteers, technology, and storytelling to improve the lives of families and address the barriers to care within marginalized communities. Their success depends on a holistic, community-centered approach that addresses three primary needs: education and training, stigma reduction, and access to care.
Challenge
The most common complication of pregnancy
PMDs are incredibly common. A reported 1 in 5 people who give birth are affected by perinatal mood disorders. This can include depression, anxiety, psychosis, obsessive-compulsive disorder, and bipolar disorder.
Multiple factors cause patients to resist seeking help. Stigma, a lack of access to behavioral health care, and poor provider training all contribute to new parents not getting the help they need. This is compounded by prejudice and bias experienced by marginalized communities like LGBTQIA+, Black, and Latinx families.
Black mothers are four times more likely to die from birth complications than white mothers, and Black babies are three times more likely to die within their first year of life than white babies. Transgender parents have trouble accessing pre- and postnatal appointments if their health insurance doesn’t allow care for their gender classification. Immigrant parents are less likely to seek preventative perinatal care. These are just a few examples of the treatment disparity that exacerbates mental illness for new parents.

In addition to the lack of access to care, not all healthcare professionals are equipped with the training and resources to help. Similar to Kimberly Wong’s experience, new dad TJ Hill sought care for severe depression after the birth of his daughter and was dismissed by trusted care providers. “I had done everything right. I reached out to all the healthcare professionals I could think of, and I still didn’t get the care that I needed.”
Solution
Approach to healing
“MMHN’s model is unique, says Kimberly Gray, director of strategic partnerships. “We’ve done a lot of work to make sure that all the trainings we provide are grounded in cultural awareness,” she says. The organization offers specialized seminars for healthcare workers, Black birth workers, and parents of diverse backgrounds.
MMHN’s digital impact
- 94 comprehensive trainings to healthcare workers and mental health providers
- 576 downloads of Queer and Trans Perinatal Mental Health Toolkit
- 10 online trainings offered including support groups, mental health screens, help for miscarriage and infant death, support for those experiencing suicidal ideations, and intersectional healthcare
- 200 in-person and virtual attendants for Legal and Ethical Dilemmas in Perinatal Mental Health Conference
- My Care App serves as a resource for new and prospective parents.
- Sana is a peer support program that reaches Spanish-speaking and Latinx families.


Through online conferences, webinars, blogs, and training toolkits, MMHN reaches thousands each year. Their cutting-edge approach not only improves care, but also educates care providers about challenging topics like intimacy and reproductive health.
Storytelling initiatives have reduced stigma and shame for LA County’s new parents and beyond. For example, Courageous Conversations reached 609 people in 2023. According to Kimberly, this has helped to build community, reduce isolation, inform care specialists, and promote healing for those recovering from mental illness. “We can create a space where people feel comfortable talking about the experience, sharing what that looks like and also feel held and supported.”
Using technology to drive awareness
Because MMHN serves partners at multiple organizations and relies on hundreds of donors and volunteers, they need assistance managing their vast network. They began working with Bonterra (Network for Good) in 2018. Prior to the partnership, emails and individualized correspondence were the organization’s main channel for connection.
They now use Bonterra for communication and outreach and gain crucial insights into how to improve operations. “We really wanted to see what the responses were from our communication,” says Kimberly. “That data has been extremely important to understand what people are most compelled by. The insights have helped inform our decision making as an organization.”
To date, MMHN has provided training to over 20,000 healthcare professionals. Kimberly says that the providers who have participated in an MMHN training report increased knowledge, comfort level, and preparedness level to identify and respond to perinatal mood disorders among their patients and clients. These providers and partners are kept in the loop with Bonterra’s fundraising and engagement software, which will enable MMHN’s future goals for expansion. MMHN hopes to double impact through expanded training, advocacy, and innovative programs in the coming years.
Impact
The path forward
MMHN’s progress since 2007 has impacted thousands of providers and families, but their mission won’t succeed without donations, volunteers, and the expertise that partners provide, says Kimberly.
“We’ve been able to reach and train tens of thousands, and that’s on a nominal budget with a small staff. For us, another 1% toward the U.S. giving GDP for perinatal health would allow us to double that impact to create more systemic change. More funding would allow us to expand our reach and influence on a broader scale. We would have a deeper ability to influence decision-making legislation at the county, state, and national levels. That will impact the care that families are able to receive.”
For parents struggling, Kimberly wants to remind them they aren’t alone. She points back to the storytelling series for evidence. As MMHN Governing Council Chair and storyteller Amber Sheikh said, “My advice is to reach out. Get the help you need. I promise it’s out there. And I’d tell them to remember, you are so worth it. Speak up when you are down.”

Work with Bonterra



